Prioritising the places and people that need it the most
(Un)healthy spaces
(Un)healthy spaces: Co-creating outdoor healthcare spaces
The project (Un)healthy spaces transforms neglected hospital grounds at the Ljubljana University Medical Centre into welcoming, restorative and accessible spaces that promote healing, reduce stress and support both patients and medical staff. Based on more than 500 insights from patients and medical staff, we turned a former smoking pavilion into an accessible oasis and a parking lot into a welcoming waiting area—providing restorative refuges for patients, staff, and visitors alike.
Slovenia
Regional
This hospital complex provides health services fir the entire western part of Slovenia
Mainly urban
It refers to a physical transformation of the built environment (hard investment)
Yes
2024-06-15
Yes
EIT Urban Mobility
No
No
As a representative of an organisation
Our project at the Ljubljana University Medical Centre (UMC)—Slovenia’s largest hospital campus—set out to transform neglected, overheated outdoor spaces into restorative, people-centered environments that enhance healing and overall well-being. With over 8,500 employees and thousands of patients, visitors, and family members using the campus daily, the need for accessible, green, and restorative spaces is critical. Yet decades of fragmented land-use planning, car-centric priorities, and underinvestment have resulted in neglected, overheated spaces that fail to meet the needs of the most vulnerable users.
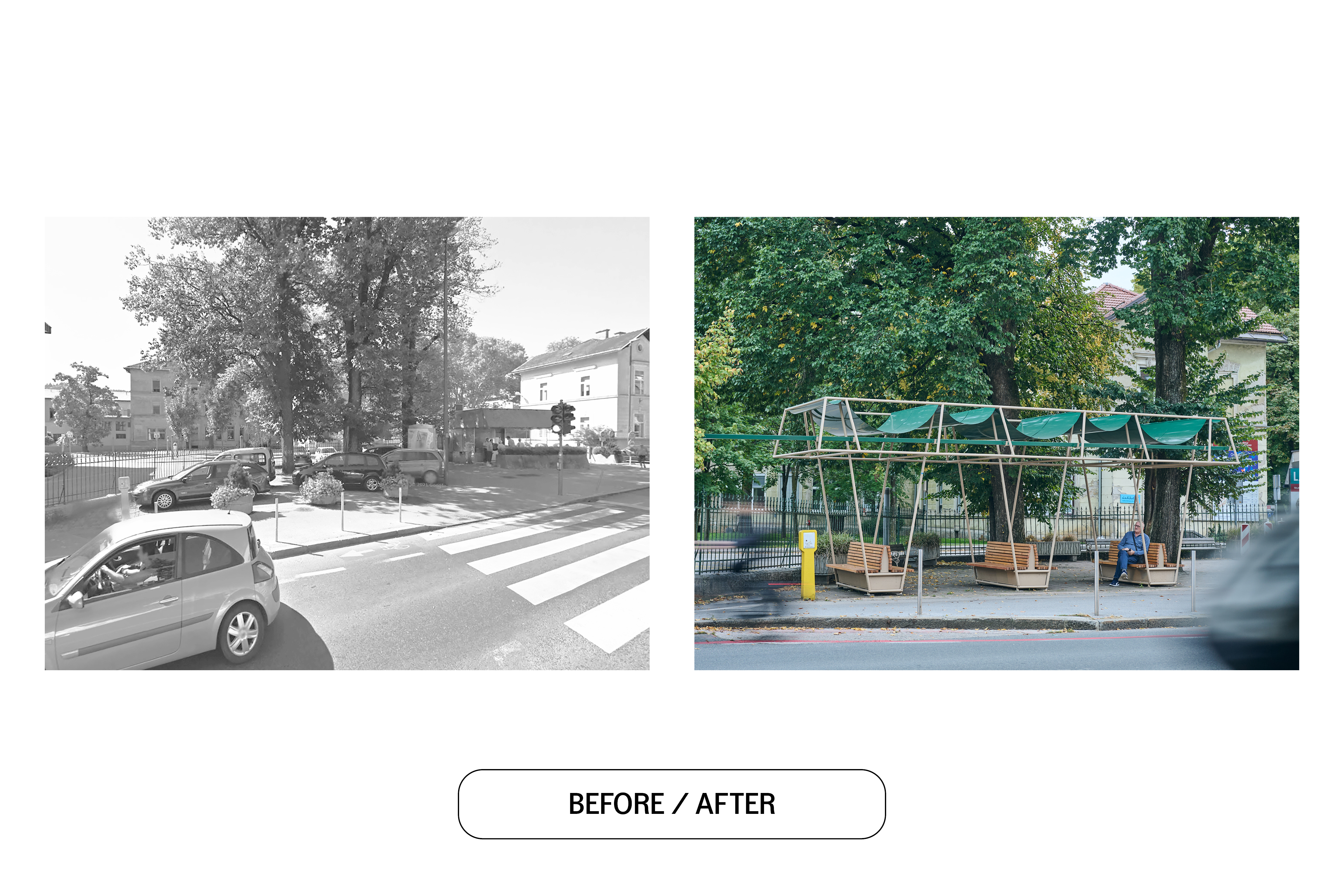
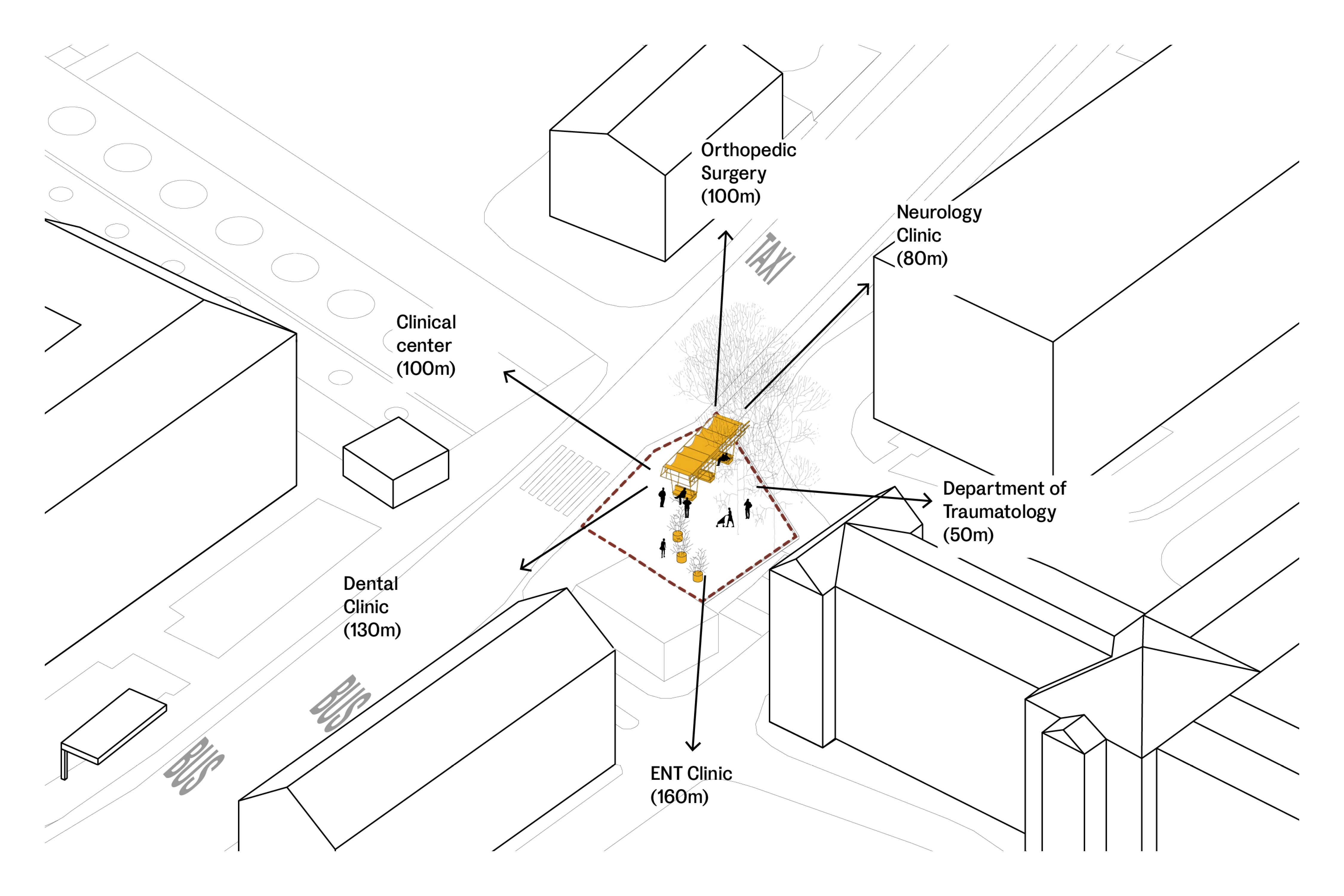
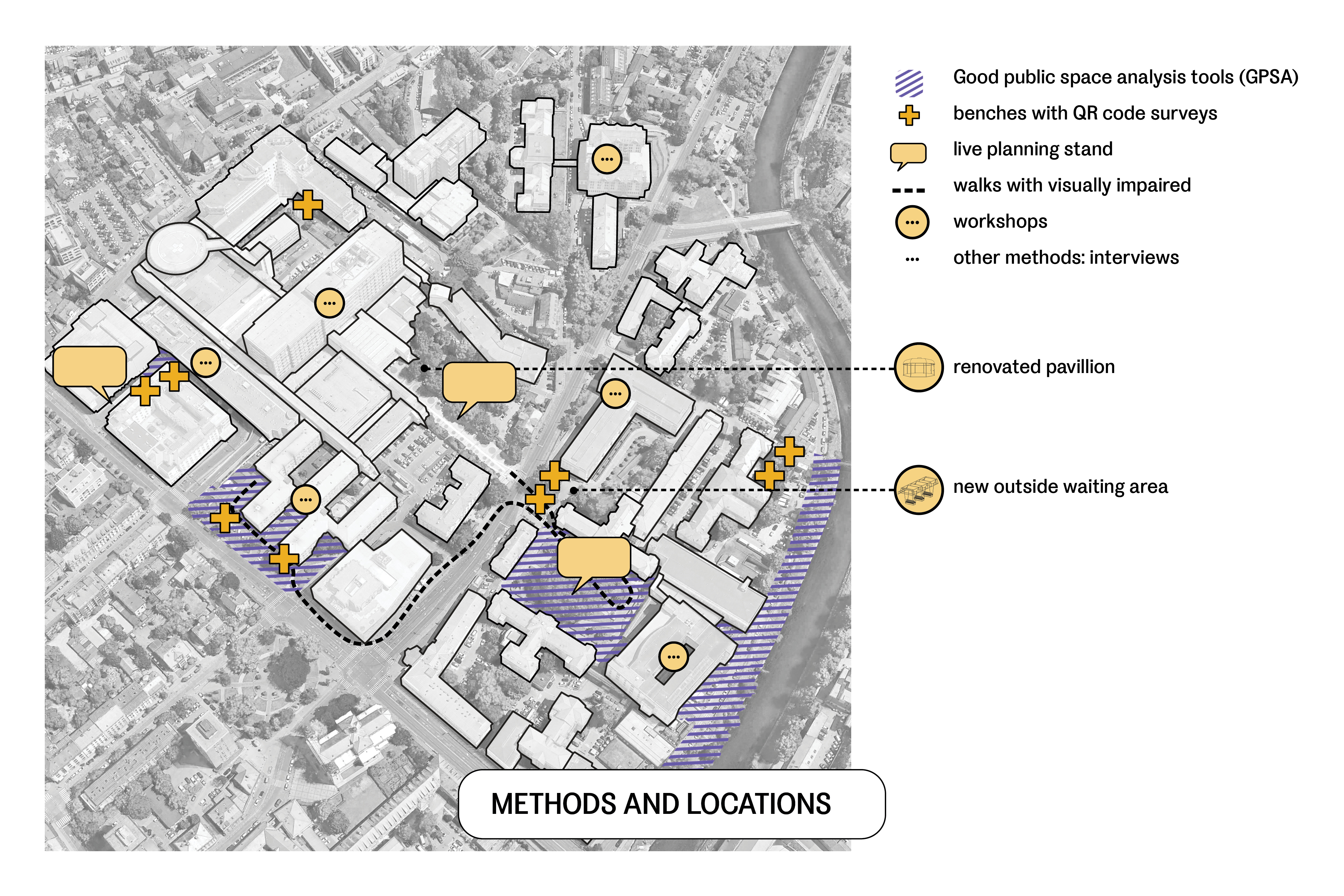
To address this, we engaged over 500 users through co-design workshops, surveys, interviews, planning stands, behavior mapping and walks with visually impaired. Their insights revealed urgent needs such as additional seating, comfortable waiting areas, improved wayfinding, and access to nature. In response, we implemented two key interventions: (1) renovation of a neglected pavilion—once used solely as a staff smoking area—into a wheelchair-accessible, nature-rich refuge, (2) repurposing VIP parking area into a new outdoor waiting zone (number one patient initiative) that provides sheltered seating in a calm, inviting setting.
User insights were translated into evidence-based design principles that now serve as a roadmap for future UMC investments, while targeted training for maintenance staff ensures the longevity and sustainability of these improvements. Our project embodies NEB values by integrating sustainability—through the protection & expansion of green spaces, aesthetics—by transforming user needs into restorative environments, and inclusion—by pioneering accessible, user-driven design. By tackling local challenges such as insufficient shade, excessive car use, poor wayfinding and fragmented public spaces, our project offers a replicable model that not only revitalizes healthcare environments but also promotes long-term community well-being across Europe.
To address this, we engaged over 500 users through co-design workshops, surveys, interviews, planning stands, behavior mapping and walks with visually impaired. Their insights revealed urgent needs such as additional seating, comfortable waiting areas, improved wayfinding, and access to nature. In response, we implemented two key interventions: (1) renovation of a neglected pavilion—once used solely as a staff smoking area—into a wheelchair-accessible, nature-rich refuge, (2) repurposing VIP parking area into a new outdoor waiting zone (number one patient initiative) that provides sheltered seating in a calm, inviting setting.
User insights were translated into evidence-based design principles that now serve as a roadmap for future UMC investments, while targeted training for maintenance staff ensures the longevity and sustainability of these improvements. Our project embodies NEB values by integrating sustainability—through the protection & expansion of green spaces, aesthetics—by transforming user needs into restorative environments, and inclusion—by pioneering accessible, user-driven design. By tackling local challenges such as insufficient shade, excessive car use, poor wayfinding and fragmented public spaces, our project offers a replicable model that not only revitalizes healthcare environments but also promotes long-term community well-being across Europe.
Healthcare outdoor spaces
Patient experience
Supportive design
Co-design
Well-being
The project integrated sustainability at multiple levels, transforming a car-dominated hospital outdoor space into a climate-adaptive, people-focused environment. The key objective was to combat the urban heat island effect—identified in the area as early as 2014—by protecting and enhancing green spaces. This was achieved through two major interventions: renovating a neglected pavilion (formerly a smoking area and informal bike parking for staff) into a calming, restorative refuge with views of nature for patients and staff, and transforming a VIP parking lot under shaded trees into a new outdoor waiting area, responding directly to patient needs about restorative spaces and places to wait outside. This waiting area was donated to UMC on the condition that the hospital prohibits parking in the space, ensuring it becomes a truly people-centered zone. By prioritizing people over cars, it turned car-dominated hospital grounds into climate-adaptive spaces.
Biodiversity enhancement was central to our approach; we incorporated native plants, permeable surfaces, and passive cooling strategies into our design principles. Sustainability was further ensured by using flexible, circular materials—such as a dismountable waiting area roof that can double as a bicycle shelter and benches that can function independently—thereby minimizing waste and maximizing adaptability. In addition, maintenance staff received targeted training to reinforce these sustainable practices, while improvements to walking infrastructure, including the removal of sidewalk barriers and strategic placement of the waiting area near a bus stop, promoted sustainable mobility and reduced reliance on private cars.
Through user-focused planning, flexible construction methods, sustainable materials and a commitment to ongoing maintenance and training, our project sets a new standard for how medical campuses can evolve sustainably while serving the diverse needs of patients, staff, and surrounding communities.
Biodiversity enhancement was central to our approach; we incorporated native plants, permeable surfaces, and passive cooling strategies into our design principles. Sustainability was further ensured by using flexible, circular materials—such as a dismountable waiting area roof that can double as a bicycle shelter and benches that can function independently—thereby minimizing waste and maximizing adaptability. In addition, maintenance staff received targeted training to reinforce these sustainable practices, while improvements to walking infrastructure, including the removal of sidewalk barriers and strategic placement of the waiting area near a bus stop, promoted sustainable mobility and reduced reliance on private cars.
Through user-focused planning, flexible construction methods, sustainable materials and a commitment to ongoing maintenance and training, our project sets a new standard for how medical campuses can evolve sustainably while serving the diverse needs of patients, staff, and surrounding communities.
Our objective was to help transform a fragmented outdoor hospital space into a cohesive, inviting environment that supports healing, recovery, and well-being for patients, staff, and visitors. By turning user insights into design principles, we set out to create long-lasting restorative, healing spaces as envisioned by those who experience them daily. Two key interventions directly responded to user needs and transformed the hospital grounds. First, a neglected pavilion—formerly closed off and used as a smoking area—was renovated into a vibrant, accessible refuge, now featuring open views of nature, added greenery, seating that offers both social interaction and quiet privacy and is accessible by a wheelchair for the first time ever, allowing all users to momentarily escape the clinical environment. Second, a new outdoor waiting area was created by repurposing an area once set aside for VIP parking. By protecting the remaining green spaces, this area not only meets the need for a covered space to wait but also helps preserve a calming, nature-centric atmosphere.
Further objective was to create a visually cohesive environment that improves wayfinding and fosters a sense of place. We standardized outdoor furniture to align with Ljubljana’s urban aesthetic and strategically placed potted flowers to guide users seamlessly from building entrances to the pavilion and waiting area. This unification of design elements addresses long-standing issues of poor navigation while reducing stress and enhancing overall well-being.
By directly integrating user feedback into every stage of the design process, our project demonstrates that modest, thoughtfully executed interventions can dramatically uplift the quality of everyday life in even the most institutional and stressful settings. It sets an exemplary model for healthcare design by proving that nature, cohesive visual elements, and user-centered insights can transform neglected spaces into vibrant, healing environments.
Further objective was to create a visually cohesive environment that improves wayfinding and fosters a sense of place. We standardized outdoor furniture to align with Ljubljana’s urban aesthetic and strategically placed potted flowers to guide users seamlessly from building entrances to the pavilion and waiting area. This unification of design elements addresses long-standing issues of poor navigation while reducing stress and enhancing overall well-being.
By directly integrating user feedback into every stage of the design process, our project demonstrates that modest, thoughtfully executed interventions can dramatically uplift the quality of everyday life in even the most institutional and stressful settings. It sets an exemplary model for healthcare design by proving that nature, cohesive visual elements, and user-centered insights can transform neglected spaces into vibrant, healing environments.
The project’s core objective was to ensure that outdoor health spaces are fully accessible to all users, particularly individuals with reduced mobility, sensory impairments, and other vulnerabilities—a need our user-experience research made abundantly clear. In response, we transformed a previously enclosed, uninviting pavilion, once used solely for staff smoking, into an inclusive space open to everyone. This renovation marked the first time that wheelchair users could access the pavilion. Additionally, we reclaimed a space formerly used for car parking to create a new covered waiting area, and turning it into an inviting spot for anyone waiting for transport or simply seeking a moment of rest. These improvements have fostered a more inclusive environment for patients—both inpatients and outpatients—staff, and visitors alike.
Recognizing that healthcare professionals, patients, and their relatives are seldom involved in discussions about their surroundings, we set a second objective: to open the decision-making process to these key stakeholders. To achieve this, 534 end-users contributed their insights through surveys, outdoor planning sessions, interviews, guided walks, and workshops. We ensured broad participation by personally inviting all known Slovenian patient associations, posting information throughout UMC, placing QR codes on benches, and running planning stands for those less comfortable with digital tools. By remaining flexible, we maximized input from both staff and patients, and their feedback was consolidated into principles of design that will inform future hospital investments.
By shifting decision-making power to those who use these spaces daily, our project offers a scalable model for participatory healthcare planning. The enhanced outdoor areas are now more welcoming and functional for users of all abilities, ages, and backgrounds, embedding co-design and shared governance into the institution’s long-term developmental strategies.
Recognizing that healthcare professionals, patients, and their relatives are seldom involved in discussions about their surroundings, we set a second objective: to open the decision-making process to these key stakeholders. To achieve this, 534 end-users contributed their insights through surveys, outdoor planning sessions, interviews, guided walks, and workshops. We ensured broad participation by personally inviting all known Slovenian patient associations, posting information throughout UMC, placing QR codes on benches, and running planning stands for those less comfortable with digital tools. By remaining flexible, we maximized input from both staff and patients, and their feedback was consolidated into principles of design that will inform future hospital investments.
By shifting decision-making power to those who use these spaces daily, our project offers a scalable model for participatory healthcare planning. The enhanced outdoor areas are now more welcoming and functional for users of all abilities, ages, and backgrounds, embedding co-design and shared governance into the institution’s long-term developmental strategies.
Citizens played a central role in shaping the project from the very beginning. Recognizing that healthcare workers, patients, and visitors are the primary users of the Ljubljana University Medical Centre’s outdoor spaces—and that nearly every citizen will interact with these areas at some point as it is the biggest Slovenian hospital and one of the biggest in Central Europe—we designed our approach to actively capture their experiences and needs. Over 8,500 employees work at UMC, and thousands more patients and visitors pass through daily. Despite this immense human traffic, the outdoor spaces remained neglected and unwelcoming - to address this gap, we engaged directly with the people most affected through a multi-method user-experience study.
We began by conducting extensive behavioral observations using the Good Public Space Tool, monitoring 583 users to understand how they navigated within key areas. This quantitative data was enriched with qualitative insights from 534 users, gathered via in-depth interviews, surveys, planning stands, targeted workshops, and a dedicated walk with visually impaired. This inclusive process enabled us to develop evidence-based design principles, which now serve as a roadmap for future investments and long-term maintenance. The direct involvement of citizens ensured that our interventions were truly responsive to their needs. Their feedback directly informed the renovation of a neglected pavilion—transformed into a welcoming, wheelchair-accessible refuge—and the creation of a new outdoor waiting area.
By involving citizens in a democratic decision-making process, the project not only produced tangible improvements on-site but also empowered the community to drive meaningful change. This collaborative process has redefined how public spaces can support well-being and sets a replicable example of how civil society involvement can transform neglected environments into places that truly prioritize comfort, accessibility, and health.
We began by conducting extensive behavioral observations using the Good Public Space Tool, monitoring 583 users to understand how they navigated within key areas. This quantitative data was enriched with qualitative insights from 534 users, gathered via in-depth interviews, surveys, planning stands, targeted workshops, and a dedicated walk with visually impaired. This inclusive process enabled us to develop evidence-based design principles, which now serve as a roadmap for future investments and long-term maintenance. The direct involvement of citizens ensured that our interventions were truly responsive to their needs. Their feedback directly informed the renovation of a neglected pavilion—transformed into a welcoming, wheelchair-accessible refuge—and the creation of a new outdoor waiting area.
By involving citizens in a democratic decision-making process, the project not only produced tangible improvements on-site but also empowered the community to drive meaningful change. This collaborative process has redefined how public spaces can support well-being and sets a replicable example of how civil society involvement can transform neglected environments into places that truly prioritize comfort, accessibility, and health.
The project engaged a diverse range of stakeholders at local, regional, and national levels, each playing a pivotal role in transforming the hospital’s outdoor spaces. At the national and regional level, the Ministry of Health—through its ownership of the UMC—provided essential oversight, while key UMC departments such as Investments, Maintenance, and Public Relations facilitated permits, helped keep staff informed about the project, and ensured strategic alignment. Locally, the City of Ljubljana, which co-owns sections of the hospital grounds, co-funded new benches and streamlined permit processes for the waiting area.
During the project, collaboration between UMC and the City of Ljubljana proved pivotal. We organized a joint meeting focused on the new waiting area, marking one of the first instances where the municipality and the hospital meaningfully coordinated their efforts. This breakthrough not only paved the way for future health-focused initiatives but also demonstrated how shared goals—such as reducing car dominance and enhancing accessibility—can unite municipal and institutional agendas.
Equally important were the hands-on local contributions of medical professionals, patients, and relatives, as well as the input of advocacy groups. Over 500 end-users participated in workshops, surveys, interviews, and guided walks, lending their real-world perspectives on challenges ranging from insufficient seating to confusing wayfinding. Their lived experiences and daily interactions with the space shaped each design solution, ensuring that enhancements addressed genuine needs. Rather than merely pointing out problems, these groups actively co-created and validated solutions, guaranteeing that interventions were both feasible and impactful. This multi-level stakeholder engagement not only resulted in tangible on-site improvements but also nurtured a culture of co-creation, shared responsibility, and open dialogue.
During the project, collaboration between UMC and the City of Ljubljana proved pivotal. We organized a joint meeting focused on the new waiting area, marking one of the first instances where the municipality and the hospital meaningfully coordinated their efforts. This breakthrough not only paved the way for future health-focused initiatives but also demonstrated how shared goals—such as reducing car dominance and enhancing accessibility—can unite municipal and institutional agendas.
Equally important were the hands-on local contributions of medical professionals, patients, and relatives, as well as the input of advocacy groups. Over 500 end-users participated in workshops, surveys, interviews, and guided walks, lending their real-world perspectives on challenges ranging from insufficient seating to confusing wayfinding. Their lived experiences and daily interactions with the space shaped each design solution, ensuring that enhancements addressed genuine needs. Rather than merely pointing out problems, these groups actively co-created and validated solutions, guaranteeing that interventions were both feasible and impactful. This multi-level stakeholder engagement not only resulted in tangible on-site improvements but also nurtured a culture of co-creation, shared responsibility, and open dialogue.
Our project integrated multiple disciplines to ensure the revitalized outdoor spaces addressed real-world needs. A psychologist guided user-experience research and facilitated workshops, creating a safe environment for discussing sensitive topics and ensuring that participants’ emotional well-being was respected. Communicology specialists helped build trust among staff in a healthcare system already under stress from strikes and organizational challenges. Maintenance staff and safety personnel provided practical insights at co-design sessions, highlighting how design solutions could be effectively maintained and secured over time. Architects and urban planners then translated user feedback—along with considerations from consultations with traffic engineers and accessibility advocates—into coherent design principles and renovation concepts, including the transformation of the pavilion and the creation of a new waiting area.
This multidisciplinary approach went beyond immediate interventions to spark knowledge exchange. We organised a public lecture featuring an international health-focused design expert from Gehl, followed by a discussion with an environmental psychologist, an occupational medicine expert, a municipal architect, and a professor of architecture. This forum highlighted the importance of stress reduction, mental health, and nature in hospital outdoor design, informing the incorporation of restorative elements into the design principles and solutions. Policy experts and municipal representatives linked these localized changes to larger agendas on climate adaptation, healthcare reform, and urban development, ensuring the project’s impact was both holistic and scalable. The added value of this interdisciplinary process lay in weaving together diverse professional insights, ensuring that each design decision served not just aesthetic or functional goals, but also user well-being, environmental resilience, and long-term institutional strategy.
This multidisciplinary approach went beyond immediate interventions to spark knowledge exchange. We organised a public lecture featuring an international health-focused design expert from Gehl, followed by a discussion with an environmental psychologist, an occupational medicine expert, a municipal architect, and a professor of architecture. This forum highlighted the importance of stress reduction, mental health, and nature in hospital outdoor design, informing the incorporation of restorative elements into the design principles and solutions. Policy experts and municipal representatives linked these localized changes to larger agendas on climate adaptation, healthcare reform, and urban development, ensuring the project’s impact was both holistic and scalable. The added value of this interdisciplinary process lay in weaving together diverse professional insights, ensuring that each design decision served not just aesthetic or functional goals, but also user well-being, environmental resilience, and long-term institutional strategy.
What distinguishes this project from mainstream hospital design is its unwavering commitment to evidence-based approach, combined with an agile, user-driven methodology that is rarely seen in such complex public healthcare settings. Research shows that integrating nature and positive distractions into hospital environments can lower stress levels, reduce the need for pain medication, and even shorten hospital stays. Yet these benefits are overlooked due to cost pressures, institutional rigidity, or lack of awareness. By contrast, this project placed user feedback at the center of every decision, ensuring that patients’ and staff’s real-world needs shaped both short-term interventions and long-term goals.
We adopted an adaptive, iterative approach to gathering and acting on feedback. A psychologist advised on how to conduct workshops and interviews sensitively, respecting the emotional states of participants—many of whom were already under significant stress due to illness or heavy workloads. When initial interviews revealed that patients had nowhere to sit, the team moved beyond standard research protocols by donating benches equipped with QR codes, enabling the quick collection of additional insights. Workshops and surveys soon revealed a lack of shelter from weather extremes, prompting the creation of a new covered waiting area.
In a sector often bogged down by bureaucracy and budgetary constraints, these flexible, bottom-up actions exemplify a new approach. The renovation of a previously inaccessible pavilion and the strategic placement of a covered waiting area between clinics were achieved with unprecedented speed—further proof that user-centric solutions can be fast-tracked even in large, public hospital complexes. This outcome underscores the project’s transformative potential, demonstrating that real-time adaptation and genuine co-creation can catalyze systemic change, boost staff morale, and significantly improve patient experiences.
We adopted an adaptive, iterative approach to gathering and acting on feedback. A psychologist advised on how to conduct workshops and interviews sensitively, respecting the emotional states of participants—many of whom were already under significant stress due to illness or heavy workloads. When initial interviews revealed that patients had nowhere to sit, the team moved beyond standard research protocols by donating benches equipped with QR codes, enabling the quick collection of additional insights. Workshops and surveys soon revealed a lack of shelter from weather extremes, prompting the creation of a new covered waiting area.
In a sector often bogged down by bureaucracy and budgetary constraints, these flexible, bottom-up actions exemplify a new approach. The renovation of a previously inaccessible pavilion and the strategic placement of a covered waiting area between clinics were achieved with unprecedented speed—further proof that user-centric solutions can be fast-tracked even in large, public hospital complexes. This outcome underscores the project’s transformative potential, demonstrating that real-time adaptation and genuine co-creation can catalyze systemic change, boost staff morale, and significantly improve patient experiences.
Although healthcare professionals, patients and their relatives are the primary users of hospital outdoor spaces, they are rarely involved in designing them. Our project aimed to change that by exploring their experiences through a multi-method user research. We observed 583 users using the Good Public Space Tool and conducted 7 in-depth interviews with medical staff to identify issues such as insufficient seating. As a response, and to gather real-time feedback, we donated 14 benches and 2 tables to UMC, equipped with a QR code linking to an open-ended survey, which 373 participants completed. For those less comfortable with digital tools, a three-day planning stand engaged 113 passersby, and we organized a walk with 15 visually impaired users to identify barrier-related challenges. Additionally, 5 targeted workshops were held—two with patient association representatives (oncology, deaf communities, tetraplegic support, dementia, fibromyalgia, etc.) and three with UMC personnel—designed to fit around busy schedules without disrupting critical services.
Directly responding to the feedback, we renovated a neglected pavilion into a welcoming, wheelchair-accessible refuge, and created a new outdoor waiting area that provides shelter and comfort. To ensure long-term impact, we educated maintenance staff through specialized workshops and held a public lecture to engage the urban planning community. The insights informed a set of evidence-based design principles for outdoor hospital spaces. We also adapted our findings into a specialized questionnaire for primary healthcare settings.
Overall, this inclusive, iterative methodology provided both immediate fixes and long-term strategies. By truly listening to the voices of those who use these spaces every day, our approach not only improves the user experience at UMC but also offers a replicable model for creating healthier, more accessible environments in healthcare facilities worldwide.
Directly responding to the feedback, we renovated a neglected pavilion into a welcoming, wheelchair-accessible refuge, and created a new outdoor waiting area that provides shelter and comfort. To ensure long-term impact, we educated maintenance staff through specialized workshops and held a public lecture to engage the urban planning community. The insights informed a set of evidence-based design principles for outdoor hospital spaces. We also adapted our findings into a specialized questionnaire for primary healthcare settings.
Overall, this inclusive, iterative methodology provided both immediate fixes and long-term strategies. By truly listening to the voices of those who use these spaces every day, our approach not only improves the user experience at UMC but also offers a replicable model for creating healthier, more accessible environments in healthcare facilities worldwide.
A key replicable aspect of this project lies in its adaptable, user-focused methodology. Rather than relying solely on conventional surveys and interviews, we employed various engagement tactics—such as QR codes on benches, flexible on-site workshops and outside planning stands—to capture insights from people who might otherwise be reluctant or unable to participate. The project’s flexible scheduling of workshop sessions demonstrated that meaningful input can be gathered without disrupting the demanding schedules of medical professionals—a strategy that could benefit any context where participants face time constraints. Equally important are the educational training sessions for maintenance staff - by equipping them with knowledge about upkeep strategies, user-centered design principles, and the importance of routine repairs, we established a sustainable maintenance model that other institutions can adopt. This inclusive, low-pressure strategy is easily transferable to other health or social care settings, from retirement homes to community clinics, and can be tailored to address different forms of vulnerability.
The experiences uncovered by this inclusive approach, from the need for private nooks for emotionally distressed patients to sheltered waiting areas for visitors, illustrate universal issues that can be addressed in various healthcare contexts. We developed guiding principles on hospital outdoor design as well as a tailored questionnaire suited for primary healthcare centers. Applying these tools has already prompted over €20,000 in municipal investment for covered seating, drop-off zones, and increased greenery in Ljubljana’s primary healthcare settings, demonstrating their applicability well beyond a single hospital campus. Such evidence-based, user-centered insights, methods, principles and solutions can yield immediate, high-impact improvements for both patients and staff, offering a scalable blueprint for institutions worldwide.
The experiences uncovered by this inclusive approach, from the need for private nooks for emotionally distressed patients to sheltered waiting areas for visitors, illustrate universal issues that can be addressed in various healthcare contexts. We developed guiding principles on hospital outdoor design as well as a tailored questionnaire suited for primary healthcare centers. Applying these tools has already prompted over €20,000 in municipal investment for covered seating, drop-off zones, and increased greenery in Ljubljana’s primary healthcare settings, demonstrating their applicability well beyond a single hospital campus. Such evidence-based, user-centered insights, methods, principles and solutions can yield immediate, high-impact improvements for both patients and staff, offering a scalable blueprint for institutions worldwide.
Healthcare systems worldwide are facing a “polycrisis,” marked by underinvestment, spatial constraints, staff burnout and shortages, and shifting mobility habits—pressures that are especially visible in large public hospitals like the UMC. Over decades, makeshift expansions and increasing parking demands have supplanted once-green areas with concrete, amplifying urban heat island effects and leaving patients, staff and visitors without comfortable outdoor spaces. Mirroring global trends of “welfare residualisation,” where austerity pressures overshadow user-centered design, Slovenia’s largest hospital faces strikes, privatization of services, and lengthy wait times—conditions worsened by the COVID-19 pandemic, which underscored the critical need for safe outdoor spaces.
In response, our project provides a local solution that addresses these challenges through local, user-driven interventions that are both low-cost and high-impact. By transforming car-dominated zones into people-focused places, we’ve introduced green covered waiting areas to alleviate overheating, enhance comfort, and support health equity. The project’s co-design process helps counteract disengagement often found in underfunded public services: user-driven feedback steers real, practical changes—such as redesigning a neglected pavilion and converting parking areas into restorative green spaces. While these interventions are relatively simple, they can reduce anxiety, shorten hospital stays, lower personnel turnover and restore a sense of dignity to care. For sustained impact, we trained maintenance staff and developed guidelines for nurturing and expanding green areas. While our efforts do not replace the need for larger-scale reforms, they show how targeted improvements can provide immediate relief in an overburdened system that often directs public funding to the cheapest rather than the most beneficial solutions.
In response, our project provides a local solution that addresses these challenges through local, user-driven interventions that are both low-cost and high-impact. By transforming car-dominated zones into people-focused places, we’ve introduced green covered waiting areas to alleviate overheating, enhance comfort, and support health equity. The project’s co-design process helps counteract disengagement often found in underfunded public services: user-driven feedback steers real, practical changes—such as redesigning a neglected pavilion and converting parking areas into restorative green spaces. While these interventions are relatively simple, they can reduce anxiety, shorten hospital stays, lower personnel turnover and restore a sense of dignity to care. For sustained impact, we trained maintenance staff and developed guidelines for nurturing and expanding green areas. While our efforts do not replace the need for larger-scale reforms, they show how targeted improvements can provide immediate relief in an overburdened system that often directs public funding to the cheapest rather than the most beneficial solutions.
Our project yielded immediate, tangible results by transforming two previously under-maintained areas into welcoming outdoor health environments. A neglected staff smoking pavilion was renovated into a wheelchair-accessible, nature-rich refuge, while a formerly car-dominated space was repurposed to create a new outdoor waiting area that offers sheltered seating and a calming environment.These enhancements directly benefit vulnerable patients in need of privacy and respite, as well as healthcare workers seeking relief from high-stress conditions. They provide a crucial counterbalance to the hospital’s clinical atmosphere, offering spaces for emotional release, social interaction, and quiet reflection that help alleviate stress and foster a sense of well-being.
The initiative also empowered users and influenced institutional policy. Through a multi-method research approach engaging 534 participants, we were able to gather diverse insights and develop evidence-based design principles that now guide future UMC outdoor renovations. These findings were further refined into a specialized questionnaire for primary healthcare settings, which has already spurred over €20,000 in municipal investments for additional greenery, seating, and improved drop-off zones.
By converting neglected areas into user-friendly, restorative spots, the project demonstrates that relatively modest interventions can substantially improve daily life in a resource-constrained healthcare environment. The Association of Slovenian Architects has recognized the value of these findings, incorporating them into official planning documents for a forthcoming medical campus. Additionally, targeted training for maintenance staff in user-centered design and sustainable upkeep ensures that these improvements remain effective and enduring.
Taken together, these results, outcomes, and impacts underscore how small-scale, cost-effective measures can yield profound benefits for the most vulnerable hospital users.
The initiative also empowered users and influenced institutional policy. Through a multi-method research approach engaging 534 participants, we were able to gather diverse insights and develop evidence-based design principles that now guide future UMC outdoor renovations. These findings were further refined into a specialized questionnaire for primary healthcare settings, which has already spurred over €20,000 in municipal investments for additional greenery, seating, and improved drop-off zones.
By converting neglected areas into user-friendly, restorative spots, the project demonstrates that relatively modest interventions can substantially improve daily life in a resource-constrained healthcare environment. The Association of Slovenian Architects has recognized the value of these findings, incorporating them into official planning documents for a forthcoming medical campus. Additionally, targeted training for maintenance staff in user-centered design and sustainable upkeep ensures that these improvements remain effective and enduring.
Taken together, these results, outcomes, and impacts underscore how small-scale, cost-effective measures can yield profound benefits for the most vulnerable hospital users.